Putting your foot down on Plantar Fasciitis – Ethan Yeung (Kinesiology UBC)
Ahh, plantar fasciitis. For those of you who’ve never had the pleasure, it isn’t a species of flower, it isn’t the name of an alien star trek antagonist, and it isn’t a sexy sounding French gourmet entree… Plantar fasciitis has an array of alia, the most common of which include: heel spur syndrome, painful heel syndrome, subcalcaneal pain, runner’s heel, calcaneal periostitis, and calcaneodynia. You can rid yourself of any notions you once had of plantar fasciitis sounding like something pleasant, just judging from the number of alternative names with the word pain in it.
What is Plantar fasciitis?
To provide you with a breakdown of the conditions name, Plantar is an anatomical term referring to the sole of the foot, Fascia are connective tissue structures that envelope individual muscles, groups of muscles, and blood vessels, binding together structures as well as providing a surface for minimal frictional sliding of other structures, and the suffix “itis” is indicative of inflammation. The name in its entirety describes a condition where one will have inflammation within the connective tissue structures at the sole of the foot.
The white strip attaching to the calcaneus and spanning the sole of the foot in the illustration below is known as the plantar fascia, and functions as a strong, fibrous band, providing support for the arch of your foot.
It’s when one experiences a prolonged stretching of the rather inflexible band of fascia that tears can occur, and consequently inflict pain and inflammation to the Plantar Fascia.
What are prominent symptoms of Plantar Fasciitis?
Symptoms have been characterized as a sharp, incessant stabbing sensation following one’s very first steps in the mornings, which can be ridiculously irritating and prove to be a negative impact towards your demeanour for the rest of the day…
… However, once the foot adjusts to the tension on the fascia, the pain will typically decrease. This pain is most often unilateral occurring in only foot, though there are many reported cases of bilateral pain.
What are the Causes of Plantar Fasciitis?
There are a myriad of factors that contribute to this condition and increase the likelihood of developing plantar fasciitis. Determinants appear equally a result of genetics and personal lifestyle choices. Some reasons are definitely consequences of the choices we have made and activities we partake in, while others simply boil down to our DNA.
For instance, plantar fasciitis is particularly common in runners, but also prominent in activities that place stress on the heel and adjoining tissue, such as ballet. Also, those who work in an environment where they must stand, or walk on hard surfaces for extended periods of time are likely to damage their plantar fascia, and this damage and be exacerbated when coupled with inadequate shoe support. Significant increases in body weight due to obesity, or pregnancy can bring about plantar fasciitis onset, and these are reasons that are due to decisions we’ve made about our body. Of course, no one actively participates in these activities aware that they’re going to develop these disorders, but many people who do have this disorder refuse to do anything about it. For obesity induced plantar fasciitis, clean up your eating habits, pay the gym a visit, shed the extra pounds and you’ll improve a whole lot more than just your feet.
Other factors are more predetermined or not within our control, like genetics, or the physical regression that accompanies age for instance. It is found that plantar fasciitis is most common for those between ages 40 and 60, and it is statistically determined that woman are more likely to experience this issue than men. It is possible that age plays the role of a determinant since osteoarthritis and rheumatoid arthritis (which develop with age) will increase ones chances of experiencing this condition.
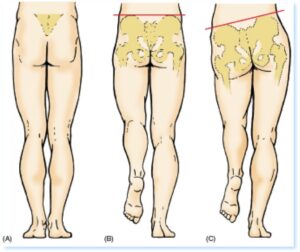 Mechanical imbalances and faulty biomechanics of the foot also have a profound influence. Studies have shown that 81%-86% of those who have symptoms of plantar fasciitis have excessive eversion of their feet. Individuals who have high arches, low arches, fallen arches, or flat feet will be at greater risk as they lack the ideal arch to most effectively intersperse tensile force during all activities, weight bearing or other.
Mechanical imbalances and faulty biomechanics of the foot also have a profound influence. Studies have shown that 81%-86% of those who have symptoms of plantar fasciitis have excessive eversion of their feet. Individuals who have high arches, low arches, fallen arches, or flat feet will be at greater risk as they lack the ideal arch to most effectively intersperse tensile force during all activities, weight bearing or other.
Furthermore, leg length discrepancies pose a greater risk of developing Plantar Fasciitis as people will often favour leaning on one leg as oppose to equally distributing their weight evenly between both, which will in turn lead to more tears and resultantly, more inflammation in plantar fascia of the shorter leg.
As amazing as it is how the musculoskeletal system works synergistically to produce movement, muscles can also affect each other negatively to produce pain. Tight calf muscles are a prime example of this tenet and are quite common in those affected by this disorder. When the calf muscles are tight, they will constantly pull the Achilles’ tendon which create more tension for the Plantar Fascia, making it more susceptible to tears.
How Can Plantar Fasciitis Be Treated?
A simple treatment is applying ice to the plantar fascia to assuage the pain and diminish inflammation. A good way to do this is to fill up a water bottle and freeze it, then to use the arch of your foot to roll the bottle back and forth.
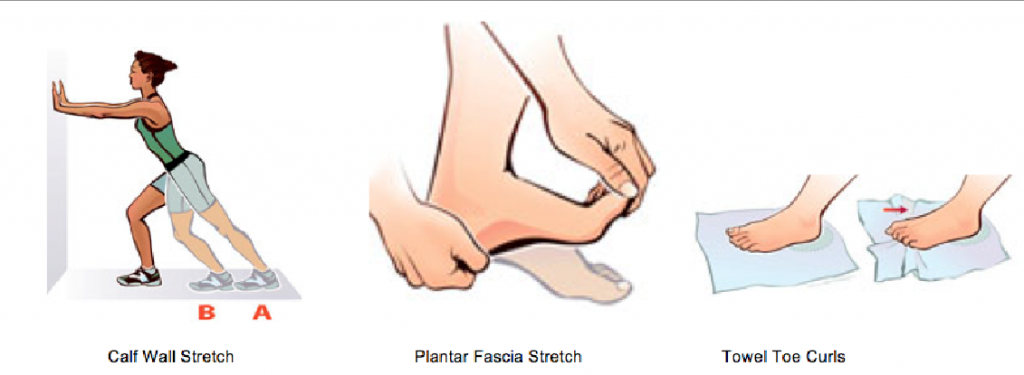
Performing and stretching the calf muscles will reduce the pull on the Achilles’ heel and reduce tension on the plantar fascia, and stretching and strengthening the supporting muscles of the foots arch will do the same. Wall calf stretches are an effective way to length the calf muscles, and stretching the fascia as shown on the right will do well to lengthen the arch supporting muscles as well as increase the flexibility of the plantar fascia. Towel curls are good for training the strength aspect of the arch muscles.
Plantar Fasciitis taping is also used to relieve pain, as well as the use of orthotics for those with flat feet, fallen arches etc. Wearing night splints will gently allow the plantar fascia and Achilles’ tendon to stretch so that they do not become overly tight through the night.
Non-steroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen (Advil, Motrin etc.) can be used as pain relief, either in pill form, or in the form of a cream that can be applied to the inflamed area of the foot, though I’d like to note that relieving effects are only temporary, and will NOT have any chronic relief.
Making lifestyle changes can be a very effective way to relieve plantar fasciitis pain, depending of course if your condition is a result of your lifestyle choice. As I said before, this could involve changing your diet and cutting down on junk food, or it could involve changing to a different kind of low-impact cardio as oppose to running, or even acquiring ample shoe support for your job that requires you to stand all day.
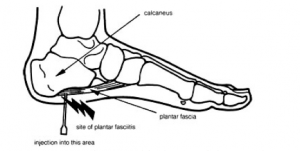 If prior more conventional treatments don’t work, a more invasive, corticosteroid injection can be administered. Though it can effectively remove the pain, there is a risk of Plantar Fascia rupture. Plantar Fasciitis rupture can entail severe pain within the arch, an initial popping sound accompanied by pain in the arch while exercising, bruising at the origin of pain, feeling a palpable mass beneath the arch, and/or no longer being able to perform a single toe raise. Treatment of this includes encasing the injured foot within a boot that will take tension off of the fascia,
If prior more conventional treatments don’t work, a more invasive, corticosteroid injection can be administered. Though it can effectively remove the pain, there is a risk of Plantar Fascia rupture. Plantar Fasciitis rupture can entail severe pain within the arch, an initial popping sound accompanied by pain in the arch while exercising, bruising at the origin of pain, feeling a palpable mass beneath the arch, and/or no longer being able to perform a single toe raise. Treatment of this includes encasing the injured foot within a boot that will take tension off of the fascia,
Prevention is always better than cure! If you haven’t already experienced the aching affliction that IS Plantar Fasciitis, and would like to remain that way, take precautionary measures. Take care of your body, and don’t over exert your fascia if you can help it. If you’re an avid runner, then invest in orthopedic support, or allow your muscles sufficient rest to prevent constantly straining your fascia. If you currently are suffering from plantar fasciitis, it is important to talk with your doctor and trusted health care team (like your kinesiologists!) about your situation, and work with them to come up with an effective action plan. Rest will be an important part of that plan (and we know those of you training for an event, or just love being on your feet will hate this advice)! But if get a good recovery plan on track ASAP, you’ll be back training and doing what you do best, pain free, in no time!